One of the most frequent dental procedures and probably one that causes us more fear. Because it is considered something complex, painful, or simply a root canal treatment. The fact of the matter is that a root canal saves your tooth and avoids extraction, although some people feel anxiety about this pain-relieving procedure. Knowing the science of root canal treatment, can take some of the mystery out and help reduce any fear. To be more qualified, the following guidance will ascertain what goes on in a root canal operation together with the science behind it and also why It is essential for an individual’s dental well-being.
1. What is Root Canal Treatment?
Root canal therapy, also known as endodontic treatment, is a dental procedure designed to eliminate infection or inflammation deep inside the soft tissue of a tooth. The pulp is the part of the tooth lying in its center that contains nerves, blood vessels, and connective tissue. The pulp can become infected if there is deep decay, cracks, or trauma which then leads to severe pain and even swelling with abscesses. Without treatment, the infection can become greater and strike surrounding tissues instead which could lead to tooth loss.
2. The Anatomy of a Tooth
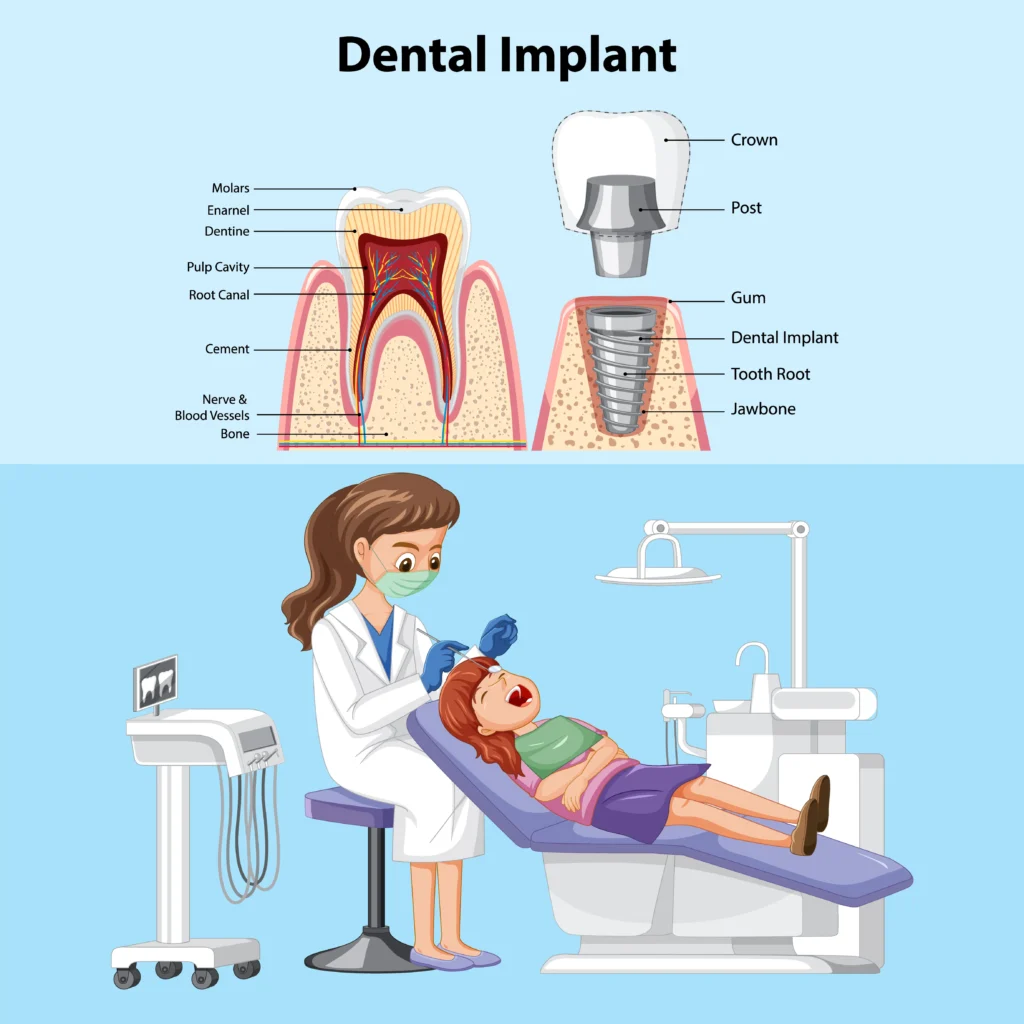
To understand how root canal treatment works, it is necessary to have a basic understanding of the anatomy of your tooth. A tooth has three layers:
The first line of protection (the hard, outermost layer) is to protect the tooth from everything. The human body consists of the hardest substance which is enamel.
- Dentin: Located just below the enamel, this layer of your tooth is less dense and can also be somewhat porous. The dentin is what relays sensations, like temperature and so forth to the pulp.
- Pulp: Tissue that contains nerves, blood vessels, and connective tissue. The vital element of the root canal tooth is that when teeth are fully formed, they can work without pulp.
3. How Does Root Can Solutions Work?
A root canal treatment is done when the pulp tissue of a tooth becomes inflamed or necrotic. There are several reasons for this:
- Advanced Cavities: Bacteria can move into the pulp as cavities progress through the dentin after passing beyond the enamel.
- Injury: An impact to the tooth that does not cause an outward crack can harm the pulp inside.
- Repetitive Dental Procedures: When a person undergoes many dental procedures on the same tooth it can further aggravate the pulp causing inflammation or infection.
- Cracks: Even the tiniest of cracks can allow bacteria to enter and infect, affecting not just tooth enamel but extending all its way through the pulp.
You can also read about Celestial Discoveries.
4. Why a Root Canal is Sometimes Necessary
Tooth Anatomy and Infection Control The definition of root canal treatment tools is designed for several key steps.
Diagnosis and preparation — step 1
The dentist would have to examine the tooth first — which may involve taking X-rays to view how large an infection is and what shape your root canals are. Inject local anesthesia into the tooth and neighboring area so that the procedure remains pain-free. The rubber dam is placed outside of the tooth so that it will not contaminate with saliva and keeps water away from the working site.
Step 2: Accessing the Pulp
The dentist numbs the area and then makes a small hole on top of that crown, to get to what counts: the pulp chamber. It is essential to get the infected or damaged tissue. Specialized dental instruments make the opening, which permits your dentist to clear up all rotors and decayed or infected material.
Stage 3: Pulpectomy or Infected Pulp Removal
The infected or inflamed pulp is carefully removed from the canal of each root while maintaining a controlled environment. This is ensured by cutting off all access to septic teeth in order not to reintroduce new bacteria into them. The process extends to the root canals, which are tiny passages that enter into a tooth from on top. Travel all of the way down until they extend out at their tips. The dentist takes special care to clean and shape these canals, removing infected tissue so they are ready to be filled.
Step 4: Disinfection
Once the pulp is removed, the inside of the tooth is cleaned and sanitized. Take this step to kill off any remaining bacteria which increases the chance of a reinfection. A process called disinfection usually achieves this by irrigating the root canals with antimicrobial solutions to clean them out.
Step 5: Filling the Canals
The dentist will clean, disinfect, and seal the tooth, then place gutta-percha, a biocompatible material, into the canals. The canals are now filled with gutta-percha, a rubber-like material that seals the area and keeps bacteria from coming back in. The dentist places a folded rubber-based sheet over your tooth during the filling process to protect its structure and maintain its chewing function without pulp.
Step 6: Sealing the Tooth
The dentist will then fill the root canals and seal the access opening in the crown with a temporary or permanent filling. In the majority of cases, a crown or other restoration is placed over this tooth to protect and reclaim complete functionality. This is a crucial step to protect the tooth from harm and further damage.
You can also read about Character Spotlight.
Conclusion
Root canal treatment is an extremely effective procedure that deals with the root causes of tooth pain. Infection without requiring a full extraction and knowing the process and what science allows patients to be less fearful of endodontic work. The process relieves the pain and infection. But it can also save a tooth that could lost and contribute to overall dental health in years ahead.